Stem Cell Research
Stem cells in animals are primal undifferentiated cells that retain the ability to produce an identical copy of themselves when they divide (self-renew) and differentiate into other cell types. In higher plants this function is the defining property of the meristematic cells. Stem cells have the ability to act as a repair system for the body, because they can divide and differentiate, replenishing other cells as long as the host organism is alive.
Medical researchers believe stem cell research has the potential to change the face of human disease by being used to repair specific tissues or to grow organs. Yet there is general agreement that, "significant technical hurdles remain that will only be overcome through years of intensive research."
The study of stem cells is attributed as beginning in the 1960s after research by Canadian scientists Ernest A. McCulloch and James E. Till.
Stem cells are also categorized according to their source, as either adult, embryonic, cancer or cord blood stem cells.
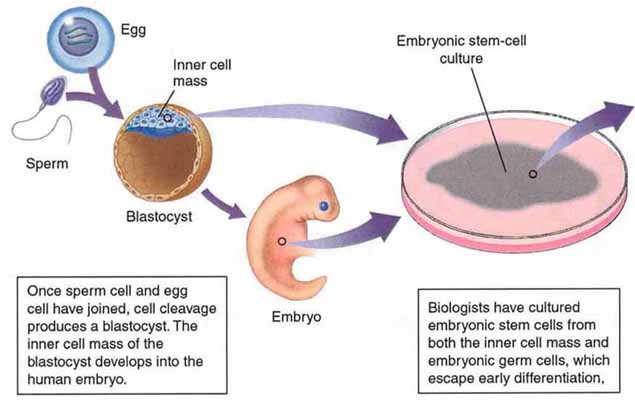
- Embryonic stem cells are cultured cells obtained from the undifferentiated inner mass cells of an early stage human embryo (sometimes called a blastocyst, which is an embryo that is between 50 to 150 cells). Embryonic stem cell research is "thought to have much greater developmental potential than adult stem cells," according to the National Institutes of Health.
Research using embryonic stem cells remains at the zenith of stem cell science because, unlike somatic cells, embryonic stem cells are pluripotent. However, research using stem cells derived from the human embryo is still in the basic research phase, as these stem cells were first isolated in 1998 (at least for humans), whereas adult stem cells have been studied since the 1960s.
Research with embryonic stem cells derived from humans is controversial because, in order to start a stem cell 'line' or lineage, the destruction of a human embryo is usually required. In an attempt to overcome these moral, political and ethical hurdles, medical researchers have been experimenting with alternative techniques of obtaining embryonic stem cells by extraction, which does not involve the cloning or destruction of a human embryo.
- Cancer stem cells arising through malignant transformation of adult stem cells are proposed to be the source of some or all tumors and cause metastasis and relapse of the disease. The stem cell origin of leukemias is well established. The role of stem cells in other tumors is under intensive investigation.
- Cord blood stem cells are derived from the blood of the placenta and umbilical cord after birth. Since 1988 these cord blood stem cells have been used to treat Gunther's disease, Hunter syndrome, Hurler syndrome, Acute lymphocytic leukemia and many more problems occurring mostly in children.
Umbilical cord blood use has become so common that there are now umbilical cord blood banks that accept donations from parents. It is collected by removing the umbilical cord, cleansing it and withdrawing blood from the umbilical vein. This blood is then immediately analyzed for infectious agents and the tissue-type is determined. The cord blood is processed and depleted of red blood cells before being stored in liquid nitrogen for later use, at which point it is thawed, washed of the cryoprotectant, and injected through a vein of the patient. This kind of treatment, where the stem cells are collected from another donor, is called allogeneic treatment. When the cells are collected from the same patient on whom they will be used, it is called autologous and when collected from identical individuals (i.e. homozygous twin), it is referred to as syngeneic.
Medical researchers believe that stem cell research has the potential to change the face of human disease. A number of current treatments already exist, although the majority of them are not commonly used because they tend to be experimental and not very cost-effective. Medical researchers anticipate being able to use technologies derived from stem cell research to treat cancer, spinal cord injuries, and muscle damage, amongst a number of other diseases, impairments and conditions. However, there still exists a great deal of social and scientific uncertainty surrounding stem cell research, which could possibly be overcome by gaining the acceptance of the public and through years of intensive research.
Stem cells however are already used extensively in research, and some scientists do not see cell therapy as the first goal of the research, but see the stem cells as a tool worthy in itself. Stem Cell ട്രീത്മെന്റ്സ്
Stem cell controversy is the ethical debate centered on research involving the creation, usage and destruction of human embryonic stem cells. Some opponents of the research argue that this practice is a slippery slope to reproductive cloning and fundamentally devalues the worth of a human being. Contrarily, some medical researchers in the field argue that it is necessary to pursue embryonic stem cell research because the resultant technologies could have significant medical potential, and that excess embryos created for in vitro fertilisation could be donated with consent and used for the research. This in turn, conflicts with opponents in the pro-life movement, who advocate for the protection of human embryos. The ensuing debate has prompted authorities around the world to seek regulatory frameworks and highlighted the fact that embryonic stem cell research represents a social and ethical challenge.
Contents |
Stem cells
Stem cells are cells that are able to differentiate into specialized cell types but also retain the ability to renew themselves through cell division. They were first identified in embryos. In an embryonic blastocyst, stem cells of the inner cell mass proceed to develop into all of the tissues and organs of the body. In adults, progenitor cells and possibly multipotent adult stem cells act as a repair system for the body, replenishing more specialized cells. The existence of truly pluripotent stem cells in adult human beings is still scientifically controversial.
Therapies
Since stem cells have the potential to be differentiated into basically any type of cell, they offer promise in the development of medical treatments for a wide range of conditions. These include damage to the brain, spinal cord, skeletal muscles and the heart. Treatments that have been proposed follow either physical trauma (e.g. spinal cord injuries), degenerative conditions (e.g. Parkinson's disease), or even genetic diseases (in combination with gene therapy). Yet further treatments using stem cells could potentially be developed thanks to their ability to repair extensive tissue damage.[1]
Much success and potential has been demonstrated from research using adult stem cells. There are no approved treatments or human trials using embryonic stem cells. Nevertheless, some are of the opinion that the differentiation potential of embryonic stem cells is broader than most adult stem cells. In addition, embryonic stem cells are considered more useful for nervous system therapies, as researchers have struggled to identify and isolate neural progenitors from adult tissues. Embryonic stem cells, however, might be rejected by the immune system - a problem which wouldn't occur if the patient received his or her own stem cells.
The major controversy is that the "best" stem cells come from growing embryos. The problem with the statement above is that the majority of the adult stem cells come from bone marrow transplants; these stem cells can help cure diseases such as leukemia, but they are not near as effective to diseases such as diabetes.
Alternative sources
Some stem cell researchers are working to develop techniques of isolating stem cells that are as potent as embryonic stem cells, but do not require a human embryo.
Some believe that human somatic cells can be coaxed to "de-differentiate" and revert to an embryonic state. Researchers at Harvard University, led by Kevin Eggan, have attempted to transfer the nucleus of a somatic cell into an existing embryonic stem cell, thus creating a new stem cell line.[2] Another study published in August 2006 also indicates that differentiated cells can be reprogrammed to an embryonic-like state by introducing four specific factors.[3]
Researchers at Advanced Cell Technology, led by Robert Lanza, reported the successful derivation of a stem cell line using a process similar to preimplantation genetic diagnosis, in which a single blastomere is extracted from a blastocyst.[4] At the 2007 meeting of the International Society for Stem Cell Research (ISSCR) [5], Lanza announced that his team had succeeded in producing three new stem cell lines without destroying the parent embryos. "These are the first human embryonic cell lines in existence that didn't result from the destruction of an embryo." Lanza is currently in discussions with the National Institutes of Health (NIH) to determine whether the new technique sidesteps U.S. restrictions on federal funding for ES cell research.[6]
According to a January 9, 2007 Daily Telegraph (London) article reporting on a statement by Dr. Anthony Atala of Wake Forest University, there is another "ethical" source of stem cells. The fluid surrounding the fetus has been found to contain stem cells, that, when utilized correctly, "can be differentiated towards cell types such as fat, bone, muscle, blood vessel, nerve and liver cells", according to the article. The extraction of this fluid does not harm the fetus in any way as well. "Our hope is that these cells will provide a valuable resource for tissue repair and for engineered organs as well," said Dr Atala.[7]
Patents
The patents covering a lot of work on human embryonic stem cells are owned by the Wisconsin Alumni Research Foundation (WARF). WARF does not charge academics to study human stem cells but does charge commercial users. WARF sold Geron Corp. exclusive rights to work on human stem cells but later sued Geron Corp. to recover some of the previously sold rights. The two sides agreed that Geron Corp. would keep the rights to only three cell types. In 2001 WARF came under public pressure to widen access to human stem-cell technology.[8]
These patents are now in doubt as a request for review by the US Patent and Trademark Office has been filed by non-profit patent-watchdogs The Foundation for Taxpayer & Consumer Rights and the Public Patent Foundation as well as molecular biologist Jeanne Loring of the Burnham Institute. According to them, two of the patents granted to WARF are invalid because they cover a technique published in 1992 for which a patent had already been granted to an Australian researcher. Another part of the challenge states that these techniques, developed by James A. Thomson, are rendered obvious by a 1990 paper and two textbooks.
The outcome of this legal challenge is particularly relevant to the Geron Corp. as it can only license patents that are upheld.[9][10]
Viewpoints
The status of the human embryo and human embryonic stem cell research is a controversial issue as, with the present state of technology, the creation of a human embryonic stem cell line requires the destruction of a human embryo. Stem cell debates have motivated and reinvigorated the pro-life movement, whose members are concerned with the rights and status of the embryo as an early-aged human life. They believe that embryonic stem cell research instrumentalizes and violates the sanctity of life and is tantamount to murder.[11] The fundamental assertion of those who oppose embryonic stem cell research is the belief that human life is inviolable, combined with the fact that human life begins when a sperm cell fertilizes an egg cell to form a single cell. (see Sexual reproduction)
A portion of stem cell researchers use embryos that were created but not used in in vitro fertility treatments to derive new stem cell lines. Most of these embryos are to be destroyed, or stored for long periods of time, long past their viable storage life. In the United States alone, there have been estimates of at least 400,000 such embryos.[12] This has led some opponents of abortion, such as Senator Orrin Hatch, to support human embryonic stem cell research.[13]
Medical researchers widely submit that stem cell research has the potential to dramatically alter approaches to understanding and treating diseases, and to alleviate suffering. In the future, most medical researchers anticipate being able to use technologies derived from stem cell research to treat a variety of diseases and impairments. Spinal cord injuries and Parkinson's disease are two examples that have been championed by high-profile media personalities (for instance, Christopher Reeve and Michael J. Fox). The anticipated medical benefits of stem cell research add urgency to the debates, which has been appealed to by proponents of embryonic stem cell research.
In August, 2000, The U.S. National Institutes of Health's Guidelines stated:
"...research involving human pluripotent stem cells...promises new treatments and possible cures for many debilitating diseases and injuries, including Parkinson's disease, diabetes, heart disease, multiple sclerosis, burns and spinal cord injuries. The NIH believes the potential medical benefits of human pluripotent stem cell technology are compelling and worthy of pursuit in accordance with appropriate ethical standards." [14]
Recently, researchers at Advanced Cell Technology of Worcester, Mass., succeeded in obtaining stem cells from mouse embryos without killing the embryos.[15] If this technique and its reliability are improved, it would alleviate some of the ethical concerns related to embryonic stem cell research.
Another technique announced in 2007 may also defuse the longstanding debate and controversy. Research teams in the United States and Japan have developed a simple and cost effective method of reprogramming human skin cells to function much like embryonic stem cells by introducing artificial viruses. While extracting and cloning stem cells is complex and extremely expensive, the newly discovered method of reprogramming cells is much cheaper. However, the technique may disrupt the DNA in the new stem cells, resulting in damaged and cancerous tissue. More research will be required before non-cancerous stem cells can be created.[16][17][18][19]
Endorsement
Utilitarianism
The benefits of stem cell research outweigh the cost in terms of embryonic life
- Embryonic stem cells have the capacity to grow indefinitely in a laboratory environment and can differentiate into almost all types of bodily tissue. This makes embryonic stem cells an attractive prospect for cellular therapies to treat a wide range of diseases.[20]
- The social, economic and personal costs of the diseases that embryonic stem cells have the potential to treat are far greater than the costs associated with the destruction of embryos.
Human potential and humanity
This argument often goes hand-in-hand with the utilitarian argument, and can be presented in several forms:
- Embryos, while of value, are not equivalent to human life while they are still incapable of existing outside the womb (i.e. they only have the potential for life).
- Approximately 18% of zygotes do not implant after conception. Thus far more embryos are lost due to chance than are proposed to be used for embryonic stem cell research or treatments.
- Blastocysts are a cluster of human cells that have not differentiated into distinct organ tissue; making cells of the inner cell mass no more "human" than a skin cell .[20]
- Some parties contend that embryos are not humans, believing that the life of Homo sapiens only begins when the heartbeat develops, which is during the 5th week of pregnancy,[21] or when the brain begins developing activity, which has been detected at 54 days after conception.[22]
Consequentialism
The ends (i.e. new treatments and cures) justify the means (i.e. the destruction of embryos)
This can be seen as a more extreme view of the utilitarianism argument.
Efficiency
If an embryo is going to be destroyed anyway, isn't it more efficient to make practical use of it?
- In vitro fertilization (IVF) generates large numbers of unused embryos (e.g. 70,000 in Australia alone).[20] Many of these thousands of IVF embryos are slated for destruction. Using them for scientific research utilizes a resource that would otherwise be wasted.[20]
- While the destruction of human embryos is required to establish a stem cell line, no new embryos have to be destroyed to work with existing stem cell lines. It would be wasteful not to continue to make use of these cell lines as a resource.[20]
- Abortions are legal in many countries and jurisdictions. A logical argument follows that if these embryos are being destroyed anyway, why not use them for stem cell research or treatments?
Superiority
Embryonic stem cells can be considered far more useful therapeutically than adult stem cells
This is usually presented as a counter-argument to using adult stem cells as an alternative that doesn't involve embryonic destruction.
- Embryonic stem cells make up a significant proportion of a developing embryo, while adult stem cells exist as minor populations within a mature individual (e.g. in every 10,000 cells of the bone marrow, only 10 will be usable stem cells). Thus, embryonic stem cells are likely to be easier to isolate and grow ex vivo than adult stem cells.[20]
- Embryonic stem cells divide more rapidly than adult stem cells, potentially making it easier to generate large numbers of cells for therapeutic means. In contrast, adult stem cell might not divide fast enough to offer immediate treatment.[20]
- Embryonic stem cells have greater plasticity, allowing them to treat a wider range of diseases.[20]
- Adult stem cells from the patient's own body might not be effective in treatment of genetic disorders. Allogeneic embryonic stem cell transplantation (i.e. from a healthy donor) may be more practical in these cases than gene therapy of a patient's own cell.[20]
- DNA abnormalities found in adult stem cells that are caused by toxins and sunlight may make them poorly suited for treatment.[20]
- Embryonic stem cells have been shown to be effective in treating heart damage in mice.[20]
Beginning of life
- Before the primitive streak is formed when the embryo attaches to the uterus at approximately 14 days after fertilization, a single fertilized egg can split in two to form identical twins. Also, rarely, two separately fertilized eggs can, instead of resulting in fraternal twins, fuse together and develop into a single human individual (a tetragametic chimera).[23]
- Therefore before the primitive streak is formed, an individual human life does not exist at fertilization, as it can go on to split into two separate individuals. Therefore, an individual human life begins when the primitive streak is formed — beyond which the cell group cannot split to make twins — and not before. Therefore the blastocysts destroyed for embryonic stem cells do not have human life, and it is ethical to use them. [23]
Objection
Value of life
An embryo is actually a human; it should be valued as highly as a human life.
The reasoning can be summed up by the fact that, once an egg is fertilized, unless inhibited, it will develop into a fully-developed adult. This opinion is often related to religious doctrines which assert that conception marks the beginning of human life or the presence of a soul. Based upon this reasoning, the subsequent argument against embryonic stem cell research is that human life is inherently valuable and should not be voluntarily destroyed.
It has been argued that "the line at which an embryo becomes a human life remains as arbitrary as ever".[24]
Viability is another standard under which embryos and fetuses have been regarded as human lives. In the United States, the 1973 Supreme Court case of Roe v. Wade concluded that viability determined the permissibility of abortions performed for reasons other than the protection of the woman's health, defining viability as the point at which a fetus is "potentially able to live outside the mother's womb, albeit with artificial aid."[25] The point of viability was 24 to 28 weeks when the case was decided and has since moved to about 22 weeks due to advancement in medical technology. If further technological advances allow a sperm and egg to be combined and fully developed completely outside of the womb, an embryo will be viable as soon as it is conceived, and under the viability standard, life will begin at conception.
Better alternatives
Embryonic stem cells should be abandoned in favor of alternatives, such as those involving adult stem cells.
This argument is used by opponents of embryonic destruction as well as researchers specializing in adult stem cell research.
It is often claimed by pro-life supporters that the use of adult stem cells from sources such as umbilical cord blood has consistently produced more promising results than the use of embryonic stem cells.[26] Furthermore, adult stem cell research may be able to make greater advances if less money and resources were channeled into embryonic stem cell research.[27]
Adult stem cells have already produced therapies, while embryonic stem cells have not.[28][29] Moreover, there have been many advances in adult stem cell research, including a recent study where pluripotent adult stem cells were manufactured from differentiated fibroblast by the addition of specific transcription factors. [30] Newly created stem cells were developed into an embryo and were integrated into newborn mouse tissues, analogous to the properties of embryonic stem cells.
This argument remains hotly debated on both sides. Those critical of embryonic stem cell research point to a current lack of practical treatments, while supporters argue that advances will come with more time and that breakthroughs cannot be predicted.
Scientific flaws
The use of embryonic stem cell in therapies may be fundamentally flawed.
For instance, one study suggests that autologous embryonic stem cells generated for therapeutic cloning may still suffer from immune rejection.[31] The researchers note that: "Our results raise the provocative possibility that even genetically matched cells derived by therapeutic cloning may still face barriers to effective transplantation for some disorders." In other words, therapeutic cloning may not always produce tissues immune to rejection. In contrast, there are reports of adult stem cells being successfully reintegrated into an autogenic animal.
Another concern with embryonic stem cell treatments is a tendency of stem cells from embryos to create tumors. [28][32]
Overstatement of research potential
Scientists have long promised spectacular results from embryonic stem cell research, and this has not yet occurred[24][33][34]
Conspicuously, such criticism has even come from researchers themselves. For example, in November 2004, Princeton University president and geneticist Shirley Tilghman said, "Some of the public pronouncements in the field of stem-cell research come close to overpromising at best and delusional fantasizing at worst."[35] Similarly, fertility expert and former president of the British Association for the Advancement of Science, Lord Winston has warned of a public backlash against stem cell research if it fails to deliver on some of the "hype" surrounding potential treatments.[36]
Policy debate in the United States
Origins
In 1973, Roe v. Wade legalized abortion nationwide. Five years later, the first successful human in vitro fertilization resulted in the birth of Louise Brown in England. These developments prompted the federal government to create regulations barring the use of federal funds for research that experimented on human embryos. In 1995, the NIH Human Embryo Research Panel advised the Clinton administration to permit federal funding for research on embryos left over from in vitro fertility treatments and also recommended federal funding of research on embryos specifically created for experimentation. In response to the panel's recommendations, the Clinton administration, citing moral and ethical concerns, declined to fund research on embryos created solely for research purposes,[37] but did agree to fund research on left-over embryos created by in vitro fertility treatments. At this point, the Congress intervened and passed the Dickey Amendment in 1995 (the final bill, which included the Dickey Amendment, was signed into law by Bill Clinton) which prohibited any federal funding for the Department of Health and Human Services be used for research that resulted in the destruction of an embryo regardless of the source of that embryo.
In 1998, privately funded research led to the breakthrough discovery of Human Embryonic Stem Cells (hESC). This prompted the Clinton Administration to re-examine guidelines for federal funding of embryonic research. In 1999, the president's National Bioethics Advisory Commission recommended that hESC harvested from embryos discarded after in vitro fertility treatments, but not from embryos created expressly for experimentation, be eligible for federal funding. Even though embryos are always destroyed in the process of harvesting hESC, the Clinton Administration decided that it would be permissible under the Dickey Amendment to fund hESC research as long as such research did not itself directly cause the destruction of an embryo. Therefore, HHS issued its proposed regulation concerning hESC funding in 2001. Enactment of the new guidelines was delayed by the incoming Bush administration which decided to reconsider the issue.
President Bush announced, on August 9, 2001 that federal funds, for the first time, would be made available for hESC research on currently existing stem cell lines; however, the Bush Administration chose not to permit taxpayer funding for research on hESC cell lines not currently in existence, thus limiting federal funding to research in which "the life-and-death decision has already been made".[38] The Bush Administration's guidelines differ from the Clinton Administration guidelines which did not distinguish between currently existing and not-yet-existing hESC. Both the Bush and Clinton guidelines agree that the federal government should not fund hESC research that directly destroys embryos.
Neither Congress nor any administration has ever prohibited private funding of embryonic research. Public and private funding of research on adult and cord blood stem cells is unrestricted.[citation needed]
U.S. Congressional response
In April 2004, 206 members of Congress signed a letter urging President Bush to expand federal funding of embryonic stem cell research beyond what Bush had already supported.
In May 2005, the House of Representatives voted 238-194 to loosen the limitations on federally funded embryonic stem-cell research — by allowing government-funded research on surplus frozen embryos from in vitro fertilization clinics to be used for stem cell research with the permission of donors — despite Bush's promise to veto the bill if passed.[39] On July 29, 2005, Senate Majority Leader William H. Frist (R-TN), announced that he too favored loosening restrictions on federal funding of embryonic stem cell research.[40] On July 18, 2006, the Senate passed three different bills concerning stem cell research. The Senate passed the first bill (Stem Cell Research Enhancement Act), 63-37, which would have made it legal for the Federal government to spend Federal money on embryonic stem cell research that uses embryos left over from in vitro fertilization procedures.[41] On July 19, 2006 President Bush vetoed this bill. The second bill makes it illegal to create, grow, and abort fetuses for research purposes. The third bill would encourage research that would isolate pluripotent, i.e., embryonic-like, stem cells without the destruction of human embryos.
In 2005 and 2007, Congressman Ron Paul introduced the Cures Can Be Found Act,[42] with 10 cosponsors. With an income tax credit, the bill favors research upon nonembryonic stem cells obtained from placentas, umbilical cord blood, amniotic fluid, humans after birth, or unborn human offspring who died of natural causes; the bill was referred to committee. Paul argued that hESC research is outside of federal jurisdiction either to ban or to subsidize.[43]
Bush vetoed another bill, the Stem Cell Research Enhancement Act of 2007,[44] which would have amended the Public Health Service Act to provide for human embryonic stem cell research. The bill passed the Senate on April 11 by a vote of 63-34, then passed the House on June 7 by a vote of 247-176. President Bush vetoed the bill on July 19, 2007.[45]
Funding
Currently, the National Institutes of Health has 399 funding opportunities for researchers interested in hESC.[citation needed] In 2005 the NIH funded $607 million worth of stem cell research, of which $39 million was specifically used for hESC.[46] Of the 514 currently recruiting clinical trials that are using stem cells as treatment, the federal government is supporting 206 of them; however, none of these trials are using hESC.[citation needed] Sigrid Fry-Revere has argued that private organizations, not the federal government, should provide funding for stem-cell research, so that shifts in public opinion and government policy would not bring valuable scientific research to a grinding halt[47]
No comments:
Post a Comment